
The rash lasts from a few hours to 2 days. Between the 2nd and 4th day of illness, the fever falls dramatically, and a rash appears (often as the fever falls) on the trunk and spreads to the limbs, neck, and face. Roseola begins with a high fever that generally responds well to acetaminophen (Tylenol). The fever may be as high as 105 degrees Fahrenheit. A fever lasting 3 (sometimes up to 7) days generally comes before the rash appears. The time between becoming infected and the beginning of symptoms (incubation period) is 5 to 15 days. It is caused by a virus called human herpesvirus 6 (HHV-6), although similar syndromes are possible with other viruses.
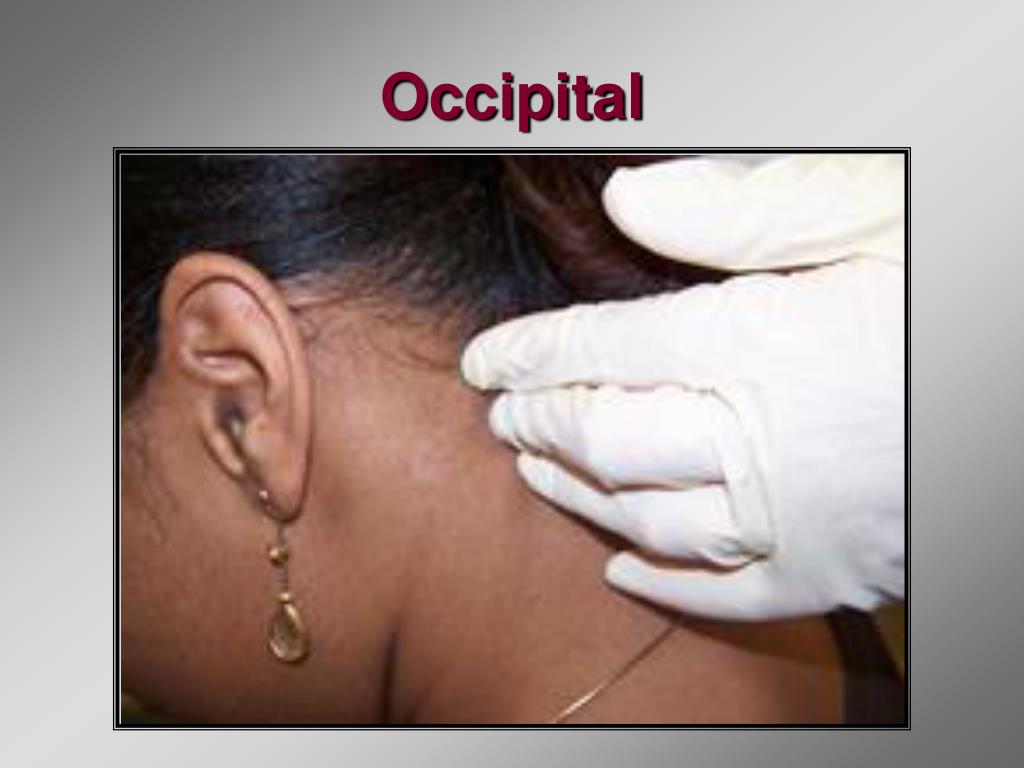
#Occipital lymph nodes update
I will update everyone on how my patient is doing as she is now taking some steroid medication and will hopefully back to her improved state within a few weeks.Definition: Roseola is an acute disease of infants and young children in which a high fever and skin rash occur.Ĭauses: The disease is common in children ages 3 months to 4 years, and most common in those ages 6 months to 1 year. If you test positive, pay attention to any neurologic symptoms and see your doctor if you are concerned. So be vigilant about your symptoms if you suspect COVID infection and get tested when you can. Since I am an optimist, while there is still much that we don’t know about acute COVID-19 infections and even less about “long-COVID”, it is also likely that like many of the respiratory symptoms, the neurologic symptoms are likely to be transient. The take home message is that neurologic symptoms are common following and during COVID infections. In fact, chronic headaches and numbness/tingling (i.e., paresthesias) were present in 68% and 60% of patients, respectively long-term. One clue might be that persistent neurologic symptoms in COVID-19 patients who never required hospitalization were present in over 50% of patients 125 days following symptoms onset. As noted above, perhaps anti-inflammatory medications might be of benefit in these cases, but currently, studies are lacking in terms of defining how long this process might last and how much medication is required. However, we don’t know exactly how the virus affects the nerves themselves although it is reasonable to postulate that COVID-19 might cause the nerves to swell such that any space around the nerve is now too small and the nerves are essentially compressed again. In fact, several post-mortem studies of patients who were infected with COVID demonstrated the presence of the virus in most brain specimens. Second, there is the possibility that the virus directly invades nerves and damages them from the inside. In this case, anti-inflammatory medications might be of benefit. This enlargement might also explain why my patient noted swelling in the back of her head. Since lymph nodes are sometimes seen near nerves, if they are enlarged, they could put pressure on those nerves and cause pain. This will cause lymph nodes to enlarge to make antibodies used to fight the viral infection. So what might be going on in those patients, specifically my patient noted above? One possible explanation is that COVID infection causes a severe, systemic inflammatory response. But thankfully, especially with the latest, Omicron variant, most people are not hospitalized. The question in my mind immediately became, “What’s the connection here between ON and COVID?” What this question is really asking is how COVID affects the nervous system.įirst, it is estimated that more than 80% of hospitalized patients will experience some type of neurologic symptoms. Within a few days, many of her headache symptoms returned, accompanied by a focal swelling in the back of the head. She was doing extremely well with “over 90% relief” at the one-year mark, when she was diagnosed with COVID-19. I was speaking with a patient of mine who was a bit more than one year out from her occipital neuralgia operation. I always knew it was just a matter of time and it finally happened.


 0 kommentar(er)
0 kommentar(er)
